
However, evidence suggests that the incidence, prevalence, and severity of many nervous system conditions (eg, stroke, neurological infections, and some mental health disorders) can be affected by climate change. The data show broad and complex adverse effects, especially of temperature extremes to which people are unaccustomed and wide diurnal temperature fluctuations. Protective measures might be possible through local forecasting. Few studies project the future effects of climate change on brain health, hindering policy developments. Robust studies on the threats from changing climate for people who have, or are at risk of developing, disorders of the nervous system are urgently needed.
Summary
Anthropogenic climate change is affecting people's health, including those with neurological and psychiatric diseases. Currently, making inferences about the effect of climate change on neurological and psychiatric diseases is challenging because of an overall sparsity of data, differing study methods, paucity of detail regarding disease subtypes, little consideration of the effect of individual and population genetics, and widely differing geographical locations with the potential for regional influences. However, evidence suggests that the incidence, prevalence, and severity of many nervous system conditions (eg, stroke, neurological infections, and some mental health disorders) can be affected by climate change. The data show broad and complex adverse effects, especially of temperature extremes to which people are unaccustomed and wide diurnal temperature fluctuations. Protective measures might be possible through local forecasting. Few studies project the future effects of climate change on brain health, hindering policy developments. Robust studies on the threats from changing climate for people who have, or are at risk of developing, disorders of the nervous system are urgently needed.
Introduction
Climate change is already challenging the health and survival of people in every country. The mean surface temperature on Earth has risen by 1·48°C since the industrial revolution started, with significant increases in the number of extreme weather events (eg, storms, droughts, heatwaves, wildfires, and floods), leading to heightened loss of life and deleterious effects on wellbeing and livelihoods globally. 2023 was the warmest year on record. Fulfilment of the nationally determined 2030 targets collated at the UN Climate Change Conference of the Parties (COP) 28 climate negotiations would still result in an average temperature rise of 2·4–2·8°C by 2100. High humidity and temperatures will extend the regions and durations of time for which normal human thermoregulatory tolerance will be exceeded outdoors. These increases in humidity and temperature are already causing considerable loss of outdoor labour and, in the future, will affect food production and security. A huge body of scientific literature now describes the potential health consequences of climate change at the population level: the number of annual heat-related deaths in adults older than 65 years increased by 85% from 1991–2000 to 2013–22, an increase that would have been 38% (due to secular changes—ie, ageing populations) if temperatures had not risen. However, detailed consideration of disease-specific effects of climate change is sparse.Neurological disorders are the leading causes of disability-adjusted life-years, are the second leading cause of death globally, and contribute substantially to societal inequalities. Mental health disorders affect over 10% of the global population; severe mental illnesses generate a mortality gap (with an average life expectancy reduction of 18 years compared with the general population). To understand effects of climate change on neurological and psychiatric disorders, we consider the literature on the neurological conditions that had the highest disease burden in order of their age-standardised disability-adjusted life-years ranking among neurological disorders in the Global Burden of Diseases, Injuries, and Risk Factors 2016 study. We also consider the effects of climate change on common psychiatric diseases, given their high incidence of comorbidity with neurological diseases. We do not include effects of pollution on neurological and neuropsychiatric diseases, as these aspects were covered in a recent review. We provide an interpreted synthesis of the published literature, emphasising the major findings, and stating the difficulties of such work and the gaps in knowledge that remain.
Effects of heating on the nervous system
Climate change has pervasive, systemic consequences. In particular, rising temperatures have health effects through multiple mechanisms, challenging the human capacity to maintain body temperature within a narrow range, which is essential to preserve vital functions (panel 1). Additionally, heat can have direct effects on molecular function, particularly that of ion channels (panel 2).
Panel 1
Effects of heat on the body
Thermoregulation requires balancing of heat loss against its generation from basal metabolism and physical activity. Elevation of skin and core temperature induces cooling through behaviour (eg, seeking shade or adjusting clothing) and physiological responses (eg, sweating or cutaneous vasodilation). When air temperature exceeds skin temperature (normally ~25–35°C), heat loss can occur only through evaporation, which is compromised as humidity rises or with activity-related heat generation. Sweat production, even in fit, acclimatised individuals, cannot exceed 3–4 L/h, limiting its thermoregulatory scope. Moreover, this sweat rate surpasses maximal enteric water absorption rate (<1·5 L/h), which increases the risk of dehydration and poses a further intrinsic limit to thermoregulatory capacity. If cooling cannot match heat generation, the resulting core temperature elevation (hyperthermia) can harm health and be fatal. Initial rises in core temperature compromise voluntary muscle activity, through effects on the CNS and peripheral nervous system and on muscles. Further core temperature elevation impairs physical function through heat cramps, caused by dehydration and electrolyte losses. Heat exhaustion (the inability to continue exercising) is more common in people who are not heat-acclimatised, and results from further dehydration, electrolyte losses, and psychological intolerance of heat. Heat exhaustion is characterised by tachypnoea, tachycardia, hypotension, cutaneous flushing, paradoxical thermal responses (eg, goosebumps and shivering), and neurological symptoms (eg, light-headedness, dizziness, headache, irritability, and lethargy). Heatstroke, a medical emergency from failed thermoregulation (ie, core body temperature >40·5°C), manifests with encephalopathy, hot dry skin, and circulatory instability; seizures, loss of consciousness, and associated circulatory collapse can be fatal, with adults older than 65 years most susceptible. Long sublethal heat exposure generates physiological adaptations, enhancing thermal tolerance; around 75% of acclimation occurs within 4–7 days, but adaptations are transient, gradually disappearing without consistent heat exposure. Heatwaves (extended periods of hot weather relative to expected local seasonal averages) can also be accompanied by high humidity, limiting heat loss from sweating and thus compounding temperature effects.
Panel 2
Temperature and ion channels
In the nervous system, the fundamental properties of signalling and communication require ion channel gating in response to electrochemical stimuli. The conformational transitions that underlie ion channel opening and closing, the balance of which determines ion flux, are typically steeply dependent on temperature. Active transmembrane transport also has high sensitivity to temperature. The extent to which nervous system complications of hyperthermia result from direct temperature effects on ion channels, synapses, and axonal function is incompletely understood. For example, the properties of voltage-gated sodium channels are influenced by temperature, a process that contributes to worsening conduction failure in demyelinating diseases with rising temperatures. Altered channel function might contribute directly to acute neurological manifestations of hyperthermia, such as seizures.
Neurological diseases, and their treatments, can undermine all aspects of thermoregulation: for example, they can compromise adaptation to long-term rising temperatures and acute temperature elevations (eg, in heatwaves). Conversely, disease pathophysiology can itself be aggravated by normal thermoregulatory responses. For most diseases, the underlying mechanisms have not yet been well studied, but there are plausible links between climate change-related drivers (eg, higher temperatures) and consequent generation or disruption of pathophysiology, based on current understanding of how heat affects the human body.
Neurological and psychiatric disorders and climate change
The scale of potential effects of climate change on neurological diseases is likely to be substantial. In the 2003 European heatwave, 14 539 excess deaths occurred in France, of which 3377 (23·2%) were due to heatstroke, hyperthermia, nervous system diseases (ICD10 codes G00–H95), or mental disorders (codes F00–F99). In this section we consider disorders to which large global disease burdens have been attributed, with details of contributing references provided in appendix 1 (p 1). Stroke
Stroke is a leading cause of death and disability worldwide. The effect of climate change on stroke is likely to be particularly important given the increasing burden of stroke-related disability in low-income and middle-income countries and its disproportionate effect on older people, who are susceptible to temperature changes through impaired temperature perception and disordered thermoregulation, comorbidities, or medication use. Climate change might influence the incidence or outcome of stroke, but data are complex and show bimodality: studies from the USA and South Korea showed an increased incidence of ischaemic stroke with increasing temperature and extremes of relative humidity; whereas, studies in Canada and Spain found increased stroke admissions with lower temperatures. Increased rates of admission, mortality, or disability for stroke have been associated with higher ambient temperatures or heatwaves in most,(but not all) studies, as have increased diurnal temperature ranges or temperature extremes. Stroke incidence has been associated with cold periods or days. Mortality and morbidity after a stroke are increased by higher temperatures.Importantly, stroke is a heterogenous disorder, due to either ischaemia (caused by atherothromboembolism, cardiac embolism, or small vessel occlusion) or intracerebral haemorrhage (caused mainly by small vessel rupture); many reports of the influence of temperature on stroke do not differentiate between stroke subtypes, which could be one reason underlying the apparently discordant results. Moreover, pre-existing cardiovascular risk factors and treatments might increase the risk of stroke associated with climatic variables. The underlying mechanisms for the association between ischaemic stroke and higher temperature and humidity extremes are not known, but might include dehydration (eg, from sweating and increased skin blood flow) that increases blood viscosity, osmolality, cholesterol concentrations, and endothelial dysfunction, which could all increase the risk of thrombosis. By contrast, low temperatures or cold periods have been most consistently linked to the risk of intracerebral haemorrhage. Higher barometric pressure might also contribute to an elevated risk of hypertensive intracerebral haemorrhage. One explanation for the observed association is that cold ambient temperatures might activate the sympathetic nervous and renin–angiotensin systems, causing short-term increased blood pressure, leading to vascular rupture. Interventions to counteract the effects of climate change will thus need to address both hot and cold extremes, in the context of existing disease characteristics and risk factors. Migraine and tension-type headache
Although some patients might overestimate the role of weather, research increasingly supports patient reports that warm temperatures trigger migraine episodes. An emergency department study found a 7·5% increased migraine admission risk per 5°C ambient temperature rise. Temperature fluctuations are also linked to migraine severity, duration, and frequency; however, studies have generally been small and are potentially underpowered to evaluate multiple weather factors, such as sunlight and pollution (which itself is worsened by climate change). Overall, worsening climate conditions (including rising temperatures, extreme weather patterns, and escalating pollution) are likely to lead to effects of two types: heightened attack frequency in people who already have migraine, and an upsurge in the overall occurrence of migraine. Effects on tension-type headache seem more complex, with some studies finding that weather changes (eg, sunshine duration and ultraviolet index) trigger attacks whereas others did not. Alzheimer's disease and other dementias
Globally, about 55 million people have dementia, with more than 60% living in low-income and middle-income countries. As populations age, these numbers are projected to increase to approximately 150 million people by 2050, with the highest rates of increase expected to be in countries experiencing the largest effects of climate change. People with dementia are exceptionally susceptible to harm from extremes of temperature (eg, heat-related illness or hypothermia) and weather events (eg, flooding or wildfires), as cognitive impairment can limit their ability to adapt behaviour to environmental changes. Reduced awareness of risk is combined with a diminished capacity to seek help or to mitigate potential harm, such as by drinking more in hot weather or by adjusting clothing. This susceptibility is compounded by frailty, multimorbidity, and psychotropic medications. Accordingly, greater temperature variation, hotter days, and heatwaves lead to increased dementia-associated hospital admissions and mortality: in New England (USA), a 1·5°C increase in the mean summer temperature increased hospital admissions associated with dementia by 12%; in Madrid (Spain), hospital admissions related to Alzheimer's disease increased by 23% after a daily temperature maximum more than 1°C higher than the heatwave threshold temperature (34°C); in England, a 4·5% increase in hospital admissions related to Alzheimer's disease was observed for each 1°C above 17°C. Effects are complex, might be bimodal, and can be influenced by local factors: some studies suggest that cooler than average temperatures, or either extreme of temperature, raises numbers of hospital admissions or deaths; cumulative exposure to extreme temperatures might also be important. Meningitis and encephalitis
The identification of climate-sensitive infections is crucial for mitigating the effects of future epidemics and pandemics. WHO lists the following as potential pandemics or pandemic organisms: SARS-CoV-2, Crimean–Congo haemorrhagic fever, Ebola virus, Marburg virus, Lassa virus, MERS-CoV, SARS-CoV-2, Nipah virus, Rift Valley fever, and Zika virus—and pathogens yet to emerge. Climate change affects the transmission of many infectious diseases by altering lifecycles and behaviours of pathogens, vectors, and non-human reservoirs. Sociodemographic consequences of climate change will influence the incidence of many infections due to migration, social disruption, famine, wars, and urbanisation, compounded by both pre-existing and aggravated inadequacies of sanitation, clean water, nutrition, and health-care provision. The latitudinal range of infections is changing: regional weather conditions related to climate change have been associated with extensive mosquito-borne disease outbreaks and the spread of tick-borne encephalitis, but causes of outbreaks typically also involve other (eg, sociopolitical or geographical) factors. The arboviruses dengue, Zika, yellow fever, and chikungunya are transmitted by Aedes mosquito species; the environmental suitability for their transmission is influenced by temperature, humidity, and rainfall, all of which are affected by climate change. Dengue virus, which can cause encephalitis or encephalopathy, is currently the fastest-spreading tropical infection. Aedes albopictus has already adapted to temperate climates and carries chikungunya and dengue virus: autochthonous transmission of both diseases has occurred in the USA and France. Zika virus infection can cause congenital microcephaly, Guillain–Barre syndrome, and meningoencephalitis, and its transmission is influenced by rainfall and temperature. West Nile virus spread has been associated in many countries with changing environments and higher temperatures in most (but not all) studies, with heatwave, drought, and urban heat island effects leading to disease occurring, or being predicted to occur, in naive populations. The ranges of Lyme disease and tick-borne encephalitis have also, and are expected to further, spread, with evidence of locality-specific effects, although more data are needed. In a nationwide study in Kazakhstan, daily rates of diagnosis of viral meningitis rose 1·05 times per 1°C increase in daily average temperature, with similar sized reductions in incidence with increased humidity. Japanese B encephalitis virus, transmitted by the Culex mosquito, is endemic in south-east Asia and the western Pacific. In more temperate Asian regions, Japanese B encephalitis is transmitted in the warm season, whereas transmission occurs year-round in the tropics. Seasonal or climate change-related temperature or rainfall variations can have a significant effect on Japanese B encephalitis infection rates, with some studies showing effects in opposite directions. Some viral infections are becoming less common, possibly due to vaccination or climate change-related changes in vectors. In northern European countries and Arctic regions, where temperature increases induced by climate change are occurring at more than twice the global rate, animal migration to the north Pole might bring new microorganisms and infections, although the human populations in these regions are small. Disease correlations can be temperature-related (eg, for borreliosis, cryptosporidiosis, and leptospirosis) or water-related (eg, for Puumala virus infection, tick-borne encephalitis, Q fever, and cryptosporidiosis). Rates of aseptic meningitis rose with higher temperature (11·4% per 1°C) in South Korean urban settings. Local heating at least partly due to climate change was associated with an increased meningitis incidence in a South African setting, which was also affected by socioeconomic and other environmental factors. Observation and modelling studies both show that the effects of climate change are complex; for example, high airborne dust concentrations or economic conditions (eg, high household occupancy) compound the risk of bacterial meningitis associated with high temperatures, and latitude-related seasonal effects (eg, wind speed or oceanic oscillations) have important local influences on the risk of disease. Combining global meningitis data with temperature variability (ie, the difference between the maximum local temperature associated with the lowest incidence of meningitis and the observed absolute maximum local temperature) showed each logarithmic unit increase in temperature variability was associated with an increased overall global meningitis risk of 4·8%; low carbon emission scenarios would be associated with significantly reduced future meningitis incidence. Epilepsy
Approximately 60 million people have epilepsy. Most epilepsies share features likely to be aggravated by climate change, such as a sensitivity to sleep deprivation as a precipitant for seizures as sleep is, and will be, compromised by climate change, especially heatwaves. Ranges of infections causing or aggravating seizures or epilepsy will probably extend under most climate change scenarios. Most studies on epilepsy are small or anecdotal. Data indicate a bimodal relationship: heatwaves have been associated with increased hospital admissions for febrile seizures or epilepsy, as have warmer days compared with colder days; other studies report an increased risk of emergency unit visits with lower temperatures or a negligible association. Higher relative humidity and lower atmospheric pressure have also been associated with increased seizure risk. Similar to many neurological diseases, epilepsy encompasses a wide variety of disorders that, despite sharing the common manifestation, are caused by various underlying mechanisms. Most reports do not take this spectrum of disease biology into account, nor the effect of climate variables on other aspects related to disease, such as the potential influence of seasonal factors on the concentration of antiseizure medication in blood, emphasising the need for more granular data. Multiple sclerosis
The prevalence of multiple sclerosis increases with (both positive and negative) latitude globally and within countries, such as the USA. Additionally, there is an association between increasing severity of multiple sclerosis and higher latitude in temperate zones, which might be caused by low ultraviolet B exposure and low vitamin D concentrations, contributing to both susceptibility and severity. However, once multiple sclerosis has developed, warmer outdoor temperature is associated with worse multiple sclerosis symptoms. Up to 80% of people with multiple sclerosis complain of heat sensitivity, with temporary exacerbation of fatigue and motor, sensory, and cognitive symptoms by elevation of skin or core temperature caused by exercise or environmental temperature increases (eg, due to heatwaves). Temperature-related symptom aggravation, known as Uhthoff's phenomenon, can follow acute temperature elevation of just 0·5°C. Temperature-related symptom worsening can cause short-lasting pseudo-relapses without neuroradiological changes. Anomalously warm weather (defined as any month >1·5°C warmer than the long-term average) was associated with increased risk of emergency hospital visits, especially in patients aged 56–64 years. Higher diurnal temperature ranges, or anomalously warm weather, increased emergency hospital attendance and admissions, but other temperature-related variables did not aggravate multiple sclerosis. In a large US study, temperature variation (measured as standard deviation of temperature) most strongly predicted increased risk of clinic visits, with an important interaction with relative humidity, and additional variation by climate zones. Subjective experience of heat and cold, mediated by discomfort and fatigue rather than actual core temperature changes, might drive intolerance of ambient temperature. Psychiatric disorders
Seasonal fluctuations in presentations of serious psychiatric illness have been recorded for centuries. Data from around the world consistently show increased acute presentations of disorders with increased ambient temperature; weaker evidence suggests that both high and low extremes in temperature could exert similar effects. Incidence, hospital admissions, and mortality risk for many mental health disorders are associated with increased ambient temperature, diurnal temperature fluctuation, or both extreme hot and cold temperatures. A few studies did not find these effects on mood disorders, and additional factors (eg, atmospheric pollution) might compound or modulate the links with temperature. Mean diurnal temperature ranges higher than 3·2°C were associated with an increased hospital admission risk for schizophrenia in Taiwan. In California (USA), a 5·6°C increase in mean apparent temperature within one day was associated with a 4·8–7·9% increase in hospital visits for any mental health disorder, self-harm, intentional injury of another person, or homicide. In Bern (Switzerland), time-series data on nearly 90 000 hospitalisations for psychiatric disorders between 1973 and 2017 showed a 4% increase for every 10°C increase in daily temperature, and a higher increase for people with developmental disorders and schizophrenia. In the USA, health insurance claims on nearly 3·5 million emergency department visits related to mental health between 2010 and 2019 showed an increase on days of extreme heat compared with other days, with an incidence rate ratio of 1·08 (95% CI 1·07–1·09) for any mental health condition. Extreme weather events (eg, winter storms, flooding, or wildfires) can lead directly to acute and chronic disorders, including anxiety, post-traumatic stress, depression, and suicidal ideation, and might even affect people who were exposed prenatally. Birth season, urban settings, pollution, local climate zone effects, reduced sunshine exposure, and humidity show complex influences on the effects of climate change on mental health. A nationally representative UK sample of people with psychosis, dementia, or substance misuse showed an overall 4·9% increase in risk of death per 1°C rise in temperature on days above the 93rd percentile of the annual temperature distribution. Temperature-related deaths in patients with severe psychiatric disorders are significantly higher than equivalent estimates in the general population, thus aggravating the excess and premature mortality already seen in people with severe psychiatric disorders.Signals from generally small studies show that many other climate-related factors might influence occurrence or worsening of psychiatric disorders too, indicating the need for comprehensive prospective studies. Other neurological disorders
For Parkinson's disease, prevalence, deaths, or disability-adjusted life-years are elevated with higher temperature and in countries with higher average temperatures and higher warming indices; however, this was not the case for motor neuron disease, which was used in one study as a comparator. Other conditions, such as the neuropathic complications of diabetes, might be aggravated by climate change. For dermatomyositis, a condition sometimes seen in neurology hospitals, diurnal temperature ranges, humidity extremes, and low temperatures were associated with increased risk of hospital attendance, each with different lag intervals, showing again the complexities of the effects of climate change on disease.Neurological disorders with early onset are especially important as children will be particularly affected by climate change, potentially compromising health and brain development in childhood and aggravating existing ill-health. Indeed, many neurogenetic and neurometabolic disorders with childhood onset are triggered or exacerbated by fever and intercurrent illness (eg, mitochondrial disorders, aminoacidopathies, organic acidurias, and GNAO1-related disease) and as such, these could possibly be worsened by climate change. For example, evidence from the European perch suggests that climate change might induce adaptive changes in mitochondria during adjustment to a warmer environment, but these changes entail an increased risk of oxidative stress; studies in patients with mitochondrial disease will be important in defining the effects of climate change on mitochondrial function, both in health and for disease. Detailed experimental studies in small groups of people have shown disordered thermoregulation, and worsening spasticity with low temperatures, in people with existing spinal cord injury. Complexities of the effects of climate change on neurological and psychiatric disorders
Despite the increasing number of publications on climate and health, we note an overall scarcity of data for neurological and psychiatric diseases (figure 1). Several factors contribute to this scarcity: interpretations are constrained by complexities, such as disease heterogeneity (eg, different types of stroke or epilepsy); effects of treatments on climate associations and the effects of climate associations on treatments; differing definitions of disease, climate measures, and reporting standards; and varying methods (eg, modelling lagged effects or not). Furthermore, there is a global disparity between regions most affected by climate change (both now and in the future) and regions in which the majority of studies are undertaken (figure 2). Given that populations around the world have undergone genetic adaptation to their local climate over millennia, there are also potential influences of individual and population genetics that are yet to be explored. Human civilisation is enormously complicated and exists within a hugely complex global ecology, which is being altered by humanity at rates faster than those seen over historic timescales; comprehension of the resulting interplay between climate change and neurological disease is challenging, especially given the poor understanding of the pathobiology of most neurological diseases. Variables that influence the effects of climate change on neurological and psychiatric disorders include: cold and hot extremes and unseasonal daily temperature excursions; urban–rural differences; the built environment; oceanic cycles; local geographies (eg, rivers and green cover); local agricultural practices and wildlife and vector changes; human behaviours (seasonal or otherwise); socioeconomic deprivation; and vaccination strategies and immunity. Interactions between multiple factors are probable—eg, for sequential weather events, drug abuse, and climate-related admissions to hospital for psychiatric disorders, or vector range extension and sociopolitical upheaval. Pollution is also likely to compound climate effects. The complexity of interactions will necessitate systems approaches for the management of neuropsychiatric conditions in the context of climate change to produce the best outcomes, capitalise on cobenefits of climate mitigation and adaptation, and avoid unintended consequences. Few studies address the considerable complexity of the effects of climate change on disease. Several potentially confounding biases apply to each study reported here (panel 3). However, bias due to researcher knowledge of patient exposures, the direction of causality, and misclassification by diseases were largely unlikely in the studies included in this paper, given the sources of data used. These considerations influence the quality of detailed conclusions drawn in most of the reviewed studies but are unlikely to call into question the underlying signals suggesting an effect of climate change, especially for disorders such as stroke and infectious diseases, for which there are large numbers of publications from different regions of the world. The risks of bias noted in panel 3 will be important to consider when future studies are designed and interpreted.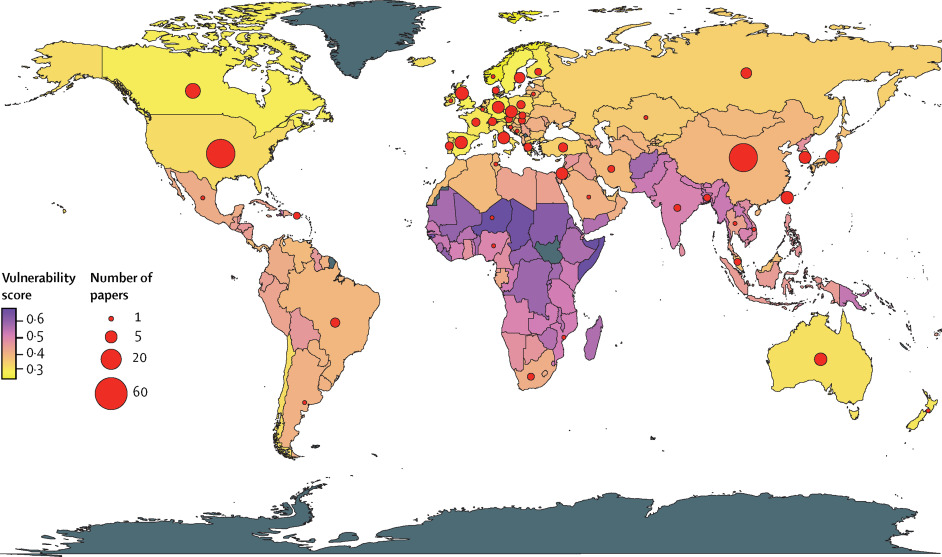
Panel 3
Risk of bias in studies included in our Personal View
-
The scarcity of individual patient-level data on weather exposure and the use of locality, rather than individual accommodation-level, climate parameters (eg, temperature and humidity and their localised sampling intervals and time-varying properties; some buildings retain heat more than others after a heatwave) can lead to mismeasurement bias
-
The scarcity of information on measures taken by patients to combat individual weather events, and their individual resources to be able to take such measures
-
Under-ascertainment and missing data due to patients not seeking medical advice for symptoms that reflect adverse health consequences of climate change (eg, increased seizure frequency), and weather events that prevent patients seeking medical attention
-
The absence of information about the weather context within which a given weather event took place (which is important, for example, as acclimation can occur after 4–7 days of exposure to higher temperatures)
Notably, studies done at different times (which sometimes have opposing findings) might not be directly comparable owing to progressive global warming between reports, with some later findings already showing differences to findings in earlier reports, in the effects of climate change. Publication bias is inevitable: diseases of economic importance in developed countries are over-represented, whereas regions of the world where people are most affected by climate change are underserved by research and health infrastructures (figure 2). Neurological research communities differ in their approaches: most studies on non-communicable diseases report climate effects on incidence, hospital admissions, or mortality, whereas neuroinfection studies concentrate on climate or seasonal effects on infection rates. Few studies address effects on patients with established neurological diseases or symptoms that occur related to climate change impacts, but that patients do not report. Data regarding the effects of heatwaves are sparse for most conditions and few global or regional studies project health outcomes within different models of climate change. Currently, there are no well established strategies for managing neurological diseases within climate change, yet health effects are probable even in heat-adapted cities, underscoring the urgent need for research and policy development. The limitations of the existing literature constrain the inferences that can be derived and, thus, the strength of the policy changes that can be advocated.
Areas for further research
Prospective, systematic, disease-focused models of how climate change projections will affect the nervous system are urgently needed. As a comparison, the SARS-CoV-2 pandemic illustrated the importance of quantitative modelling for influencing public health policies and mitigating health-care burdens. Generative modelling, originally used to estimate the spread of neuronal activity in epilepsy, was repurposed to model spread of a virus at the population level, allowing testing of hypotheses about factors underlying viral spread and pathogenicity, specifically related to temperature and seasonality. These COVID-19-related initiatives suggest that the fusion of sociobehavioural modelling, epidemiological modelling, and climate-related pathogenicity has the potential to be an important public health tool for forecasting and scenario projections. Notably, COVID-19 vaccination advice was tailored for people with neurological diseases; as projections of the effects of climate-related changes in temperature and humidity become more detailed at the local level, climate-related health projections will also need to be developed to a level of granularity that is directly useful to individuals with neurological diseases.Although meta-analyses have the capacity to offer important insights, the substantial heterogeneity, and other limitations listed previously, of existing data on neurological and psychiatric diseases make such analyses currently impossible or extremely challenging. In stroke, for which appropriate data do exist, one meta-analysis of published cohort studies (including >2 million events) reported that short-term mean ambient temperature increases were associated with increased ischaemic stroke risk (1·2% per 1°C); a meta-analysis of registry studies (476 511 participants) found no link between ambient temperature and admission for ischaemic stroke, with the authors also suggesting that increases in the preceding 24 h were more important than absolute temperature.People are already taking their own actions: caregivers of people with the rare severe epilepsy Dravet syndrome have reported that both warm weather and reduced ambient temperatures were seizure precipitants, that they would minimise exposure to warm weather (eg, through holiday locations or staying out of the sun), and that cooling measures were used (eg, by removing clothing or temporary use of portable air-conditioning units) to avoid seizures (Galia Wilson, Dravet Syndrome UK, personal communication). Anecdotally, people with some neurological diseases (eg, alternating hemiplegia of childhood, rare epilepsies, or multiple sclerosis) or their carers report rapid symptom onset soon after exposure to altered ambient temperatures, suggesting direct mediation by cutaneous sensory and effector mechanisms rather than through changes in core temperatures, which would take much longer periods of time to produce symptoms. Moreover, subjective experiences of ambient temperature might contribute to intolerance of extreme ambient temperatures. These observations require further study and might offer novel approaches for management to challenging temperature exposures.
Children are frequently listed as one of the groups most susceptible to climate change. However, as is apparent from our work (appendix 1 p 1), data specifically related to child neurological and psychiatric health in the context of climate change are particularly sparse, emphasising the need for much more research in this area, especially given that climate anxiety is highest in children and young people.Importantly, almost all the published data considered here use information on temperature gathered from weather monitoring stations that record outdoor temperature. The built environment can aggravate the effects of outdoor heat—eg, by retaining heat overnight, leading to higher night temperatures that can disrupt sleep, with attendant detrimental effects on neurological or psychiatric conditions, or by being designed for colder temperatures. Outdoor temperature recordings are likely to be particularly relevant for countries with populations that have agrarian economies, but for most high-income countries, where people typically spend most of their lives indoors, indoor temperature data will be important to collect in future studies. Emerging themes
The effects of climate change might be most marked not at absolute temperature or humidity values, but when those variables differ most (and diverge rapidly) from local historical means. People adapt to local historical climatic norms, meaning that adaptation to forecast temperature extremes in local weather might be possible; whether climate training (ie, anticipatory acclimatisation) could be beneficial and widely implemented is unknown. Other adaptations are possible: air conditioning use could help to reduce indoor temperatures but its monetary and carbon cost preclude widespread use; sustainable, passive cooling strategies include increasing urban green and blue spaces and nature-based solutions, implementation of cool, reflective roofs and pavements, and behavioural interventions (eg, avoiding direct exposure to sun, drinking more water, and wearing appropriate clothing). Climate monitoring, projection models, logic regression, and forecasting systems, identification of especially vulnerable sub-populations, and reliable warning systems for extreme weather events might reduce exposure and accompanying risks. The lag often observed between climate events and associated disease outcomes could offer a useful intervention window, as might the apparently protective effect of night-time relief from higher temperatures.The mental health consequences of climate change are important. Climate change creates new psychological challenges, notably climate anxiety, which is a chronic sense of doom related to helplessness around the climate crisis, evoking emotions including worry, fear, anxiety, grief, and anger. Worry about climate change is experienced by over two-thirds of the adult population of the USA. Although a reasonable response to climate change realities, climate anxiety can be unconstructive. People with neurological conditions are already more likely to have anxiety and depression and are more susceptible to mental health consequences of climate change than the general population. Clinical services will need to implement interventions that increase patients' perceptions of control over aspects of their disease that are within their scope of change (eg, indoor temperature control) and foster resilience skills (eg, mindfulness). Patient support organisations can engender resilience through communications that support adaptive coping and encourage activities (eg, proactive pro-environmental behaviours) to reduce anxious responses to climate change. Conclusions and future directions
Global warming mandates new approaches to nervous system diseases. People with these disorders might need to adopt behaviours to manage their condition that are new (eg, use of treatments), modified (eg, avoiding exercise during heat), intensified (eg, drinking more water), or adapted (eg, pacing of activities for fatigue). Such behaviours, and the cognitive, interpersonal, and emotional regulation skills that influence their expression, constitute changes to self-management and have the potential to reduce the effects of climate change on neurological outcomes. Carers and health-care professionals will also need to adapt how they support and manage affected individuals. Responding effectively will thus require coordination of complex interventions for people with disorders affecting the nervous system, their families, their carers, and the health and social care providers within their encompassing systems. The UK Medical Research Council recommends a systematic, theory-based and evidence-based approach to designing interventions to change self-management and practice behaviours. Use of behavioural science principles and frameworks will be essential for creating effective change.Just before COP26, 233 health journals simultaneously demanded urgent governmental action against "catastrophic harm to health" from climate change. In 2023, another powerful editorial was published across a large number of health journals and called for urgent action to tackle the global health emergency posed by the overall environmental crisis. Coordinated global action is possible, at individual and societal levels, exemplified by the SARS-CoV-2 response, for which we needed cognitive engagement (ie, individual behaviour change, modelling-led policies, and vaccine invention). Health-care professionals are trusted authorities for information about the health effects of climate change; their duty of care must encompass planning for a changing climate and advocating for health solutions. Neurologists can take action to help reduce their own effect on the climate and to provide more guidance for people with neurological disorders. Additionally, there is a pressing need for more research into the health effects of climate change on neurological and psychiatric disorders (panel 4), as recognised by funding agencies such as the Wellcome Trust and the UK Research and Innovation governmental body. Unless attention is paid to the danger to health from climate change, much of the progress that is being made in improving human health could be lost.
Panel 4
Research prioritiesMore data are needed on the effects of climate change across neurological diseases, from the individual level to the epidemiological level. This need is both urgent and challenging, as the climate continues to change, necessitating care in the interpretation of data collected during previous years, even if the relevant studies were undertaken relatively recently (eg, in the past 40 years). Responsive studies that collect data around the time of adverse weather events are challenging to organise and undertake but could quickly provide valuable information. As highlighted in this Personal View, research will also require appreciation of the complexity of the effects of climate change in a global environment that continues to warm, and will need systems thinking to ensure the multiple interacting factors that can affect disease are all considered. Most importantly, experts in specific disease areas need to engage with the concept that the effects of climate change are important in neurological and psychiatric diseases, and human health in general, and undertake relevant global transdisciplinary research that directly involves people with neurological and psychiatric conditions, and can be incorporated into global initiatives, such as the Intersectoral Global Action Plan on Epilepsy and Other Neurological Diseases.
Search strategy and selection criteria
We searched PubMed, Ovid MEDLINE, EMBASE, and PsycINFO for papers published between Jan 1, 1968, and Sept 30, 2023 that reported potential effects of extreme climate events or temperature fluctuations on 19 different nervous system conditions, chosen on the basis of the Global Burden of Disease 2016 study and supplemented by common, serious psychiatric disorders. We searched for papers on stroke, migraine and tension-type headache, Alzheimer's disease and other dementias, meningitis and encephalitis, epilepsy, multiple sclerosis, and psychiatric disorders (anxiety, depression, and schizophrenia), and other neurological conditions (Parkinson's disease, motor neuron disease, traumatic brain injury, peripheral neuropathy, myopathies, spinal cord injury, brain cancer, and tetanus), selecting those for which the paper was available as a full-text version in English, was a primary research article, provided information on extreme climate events or temperature fluctuations, and involved humans. As this topic is a new area of study, we included all studies that met the inclusion criteria, without selection based on study quality, but we note that all studies contain risks of bias, detailed in panel 3. In our main text, we focused mainly on articles published in the past 5 years about the direct aspects of climate change, further informed by a detailed review of published literature dating from 1968. Further details about our search and references we considered but that are not included in the main text can be found in appendix 2 (pp 1–2). We have grouped together migraine and tension-type headache, and meningitis and encephalitis, as from the climate change perspective the relevant studies and mechanisms are best reviewed together. Spinal cord injury, Parkinson's disease, and motor neuron disease, for which literature is sparse, are considered together under the section on other neurological conditions; for traumatic brain injury, brain and other CNS cancers, and tetanus, we found too little relevant literature to include them in this Personal View.
Contributors
SMS and MGH conceptualised the manuscript. SMS, MIG, FF, JDM, and EH undertook literature searches. MIG, FF, JDM, and EH prepared the supplementary tables and figures. SMS wrote the original draft, with contributions from EB, PC, OC, ASD, KDeM, NCF, JDW, MK, DMK, MAK, HMa, MAM, MM, HMo, MR, DJW, LZ, KJF, and MGH, who reviewed and edited the manuscript.
Declaration of interests
HMo chairs Dyson's Scientific Advisory Board and the Lancet Countdown on Health and Climate Change; holds a patent relating to a means to improve patient hydration in hospitals; is a member of the UK Climate and Health Council; is a cofounder of Real Zero (a non-profit company helping decarbonise health care); and has received honoraria for talks on climate change, but none for talks related to the topic of this Personal View. NCF is the member of the Research Strategy Council of Alzheimer's Society (UK). DJW has received grant funding from the Stroke Association and British Heart Foundation; speaking honoraria from Bayer; speaking and chairing honoraria from Alexion and NovoNordisk; and consultancy fees from Alnylam, Bayer, and NovoNordisk. DW has also participated on a data safety monitoring board for OXHARP, and the TICH-3, RESTART, MACE-ICH, and PLINTH Trial Steering Committees. MAK has received payments from Bloomsbury Genetic Therapies and PTC; holds shares in Bloomsbury Genetic Therapies (unrelated to this work as involvement pertains to the development of gene therapies for rare neurometabolic disorders); has leadership or fiduciary role in LifeArc grants committee (not relevant to this work as this membership pertains to the review of grants and allocation of funding through the Philanthropic fund); is the theme lead for the National Institute for Health Research Great Ormond Street Hospital Biomedical Research Centre Accelerating Novel Therapies; and has patents, issued or pending, for DTDS viral vector. OC reports speaking honoraria from Merck and Biogen and for participation on a data safety monitoring board for Novartis. MM has grants or contracts from Ehlers Danlos Society, Abbott, and Medtronic; reports consulting fees from AbbVie, Kriya, TEVA, Lundbeck, Eli Lilly, Salvia, and Pfizer, all paid to their institution; reports payment or honoraria for lectures, presentations, speakers bureaux, manuscript writing, or educational events from AbbVie, Pfizer, and Eli Lilly; reports patents (planned, issued, or pending) for WO2018051103A1: System and method for diagnosing and treating headaches; and is the president of the medical advisory board of CSF Leak Association and a board member of the Anglo Dutch Migraine Association. All other authors declare no competing interests.
Acknowledgments
This work was supported by the Epilepsy Society. SMS is supported by the Epilepsy Society, the National Brain Appeal Innovation Fund, and the UK Medical Research Council. NCF and MGH acknowledge support from the National Institute for Health Research University College London Hospitals Biomedical Research Centre and the UK Dementia Research Institute at University College London. KJF was funded by a Wellcome Trust Principal Research Fellowship (088130/Z/09/Z) and for the Wellcome Centre for Human Neuroimaging (205103/Z/16/Z). OC is supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre, the National Institute for Health Research, MRC, Rosetrees Trust, and the MS Society UK. EB is supported by the UK Medical Research Council (MR/W020238/1, G0901310, G1100583, and G1100583), Wellcome Trust (085475/B/08/Z and 085475/Z/08/Z), Mental Health Research UK John Grace QC award 2018, BMA Margaret Temple Fellowship, National Institute of Health Research (NIHR200756), and the National Institute for Health Research University College London Hospitals Biomedical Research Centre (Mental Health Theme). MR has research and salary support from Wellcome Trust Grant (209734/Z/17/Z). MAK has grants or contracts from NIHR Research Professorship (LifeArc/GOSHCC), Sir Jules Thorn Award for Biomedical Research, and Rosetrees Trust; and is supported by an NIHR Research Professorship and the Sir Jules Thorn Trust. HMo is supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre. MGH was supported by an Medical Research Centre strategic award to establish an International Centre for Genomic Medicine in Neuromuscular Diseases (MR/S005021/1). DMK holds grants from the Wellcome Trust and the Medical Research Council.
Source : https://www.thelancet.com/journals